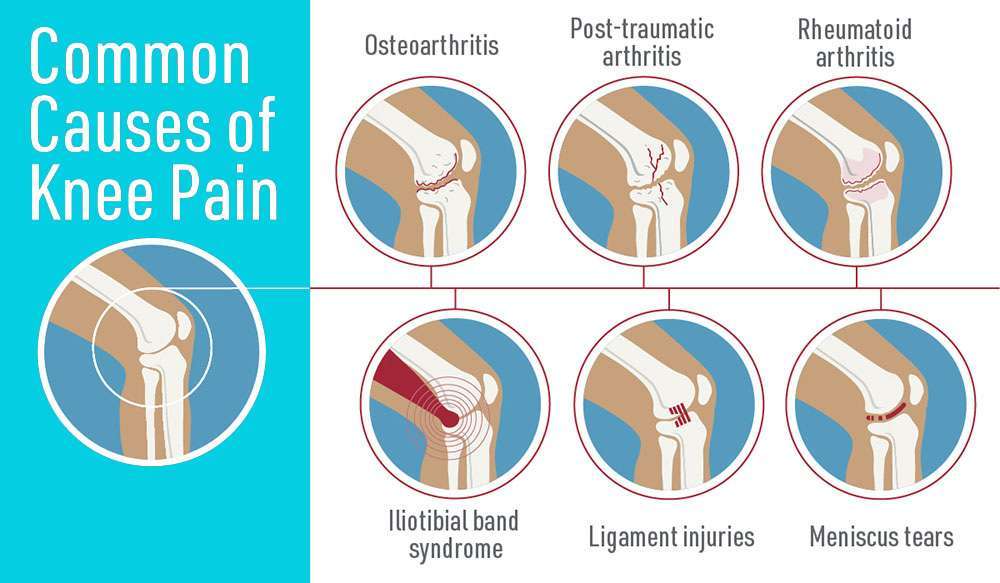
Knee pain is an extremely common injury for many people, especially athletes. The most frequent reasons for knee pain include inflamed or damaged ligaments, damage to the cartilage, and runners knee. In addition, other situations may be the reason for knee pain. These include bone chips, bursitis, and a partially dislocated kneecap. Diseases such as Iliotibial Band Syndrome, Medial Plica Syndrome, Osgood-Schlatter Disease, Osteoarthritis, and Tendonitis are also causes of knee pain. Treatments for knee pain include resting the knees, putting ice/ heat on your knee, putting a bandage around your knee to reduce swelling. Put your feet up, take non-prescription medication to reduce the swelling and practice exercises that will strengthen and stretch your knee. Please seek a doctor’s advice before attempting any exercises. Many people have had a minor knee problem at one time or another. Most of the time our body movements do not cause problems. But it’s not surprising that symptoms develop from everyday wear and tear, overuse, or injury. Knee problems and injuries most often occur during sports or recreational activities, work-related tasks, or home projects. It enables hinge and rotating movements as the connection between the upper and lower leg. This means that we can not only bend the lower leg backward but also rotate the lower leg and foot towards the upper leg. Two menisci located between the upper and lower leg bones in each knee, one on the right and one on the left side. The kneecap serves the transmission of force while extending the knee and protects the internal regions of the joint. This smooth, firm and elastic layer ensures that the knee moves easily and without friction. Both of these ligaments have significant importance for the stability of the joint. Furthermore, the medial and lateral ligaments of the knee are important for it to be precisely guided through the full range of motion of the knee. Aside from that, adequately trained muscles are quite imperative for good knee joint function. They also ensure support and stability. Muscles which are too weak often lead to knee problems.Knee joint function
News & Updates
As we age, so do our bones. There are many various types of bone pain and they can occur in all parts of the body. One pretty common type of bone pain is Pseudarthrosis. Pseudarthrosis is when the bones shift at the break point. This causes the break to not heal correctly. Some potential causes of this are smoking (nicotine can stop the capability to generate new bone), poor nutrition, aging, obesity, and osteoporosis. Other causes include diabetes, steroids, certain medicines that reduce swelling (non-steroids), not enough downtime after fusion surgery, and neck pain (some people experience no symptoms or a combination of symptoms). The pain can push out into the arms and shoulders. More inflammation & pain can develop over time by moving the neck. Diagnosis is usually confirmed with an X-ray.
Chronic pain can be caused by a single cause or a combination of causes. While each type of pain has its own origins, the following are some possible causes: Pain can occur in any diseased or traumatized tissue or organ that has nerve endings. It can also occur in the nerves themselves if they become damaged, irritated, or otherwise compromised. The following are among the more common causes/origins of chronic pain: For many people, physical pain (especially chronic pain) acts as a primary trigger for addictive behaviors. While some people may seek solace via alcohol or illegal drugs, many others start with properly prescribed medications, then develop a dependency that leads them to acquire and use these medications in improper (and, in some cases, illegal) ways. In a society in which unregulated Internet pharmacies have made acquiring prescription drugs as easy as ordering from an online catalog, it may come as little surprise that thousands of suffering Americans are attempting to self-medicate their pain away. However, as many have discovered, taking highly addictive medications without the advice or supervision of a health care provider can cause many more problems than it solves. A Jan. 4, 2008, article on the ABC News website referred to painkiller abuse as “America’s stealth addiction.” Citing statistics provided by the Department of Health and Human Services (DHHS), writer Russell Goldman noted that in 2005 the estimated number of people who used prescription painkillers for nonmedical reasons (5.2 million) was more than double the estimated 2.4 million individuals who used cocaine. Though not all of these off-label or recreational uses of prescription painkillers can be attributed to struggles with chronic pain, evidence indicates that many individuals develop dependency after using the drugs for legitimate purposes. In her article on the website of the National Pain Foundation, Dr. Jennifer P. Schneider writes that chronic pain is “notoriously under-treated,” and that the most common reasons patients gave for changing doctors included “too much pain,” and “the belief that the doctor didn’t take their pain seriously enough.” Various experts cite the following as signs that the proper use of pain-killing medication has morphed into dependency or addiction: Many pain patients have been “pre-wired” to suffer from chronic pain because of events in their lives that occurred long before the injury or event that produced the initial pain. The following are among the most Though it is common for pain patients to be described, or to describe themselves, as having become “addicted” to certain substances while attempting to ease their chronic suffering (and while some individuals do, indeed, develop addictions as a result of self-medicating), chronic pain and addiction do not always go hand-in-hand. “We treat chronic pain patients and we treat addicts who suffer from chronic pain,” one pain specialist said, noting that an improper understanding of the clinical definition of addiction results in widespread misuse of the term. “Ninety percent of chronic pain patients are actually what the literature refers to as ‘pseudo-addicts,’” he said. Whether addicted or merely dependent, pain patients who participate in an effective program will learn that the substances they are using to ease their discomfort are likely having the opposite. Most of these patients are likely to discover that their suffering subsides significantly following an initial detoxification process. Chronic Pain Treatment As indicated earlier in this document, the good news about chronic pain is that it can be effectively treated. Whether pain is caused by physical, psycho-emotional, chemical, nutritional, behavioral or environmental factors, effective treatment requires a combination of medical and psychological interventions. Treatment for chronic pain may include one or more of the following techniques: Many treatment facilities offer specialized programs for pain management. Beginning with a thorough musculoskeletal and neurological exam, pain specialists determine the origin and nature of the pain, and develop an individualized treatment plan. Essential components of treatment may include medical consultations and care, physical therapy, sensory integration, dialectical behavior therapy, trigger point therapy, acupuncture, hydrotherapy, nutrition counseling, manual therapies, and other integrative therapies. With appropriate treatment, chronic pain patients can learn to manage, control and reduce their pain. As self-awareness, mood, sleep and physical ability improve, the patient’s quality of life returns, restoring hope for an active and productive future. An effective chronic pain program should include many or all of the following elements and objectives: At Sierra Tucson, a residential recovery program in Tucson, Arizona, treatment professionals take a holistic approach to treating chronic pain that aims to restore function and improve a patient’s quality of life. By focusing on the mind, body, and spirit, patients with chronic pain can learn to accept their pain and find fulfillment in life again. “They may still experience pain every day, but it doesn’t have to ruin their lives,” said Jami Parrish, a unit therapist in Sierra Tucson’s Pain Management Program. Sierra Tucson runs the only inpatient pain program in Arizona that is accredited by the American Academy of Pain Management. In many cases, though, getting treatment for chronic pain and/or co-occurring addiction is a matter of overcoming misconceptions about the true nature of the problem. As one doctor who specializes in pain management has noted, one of the first steps in the treatment of chronic pain is to acknowledge that what the patient is experiencing is real. “Our patients come here angry and frustrated,” this doctor noted. Many chronic pain patients have been told that their conditions are “all in their heads,” or that they are exaggerating their symptoms in order to acquire prescription drugs, he added.
Chronic Pain & Substance Abuse
common risk factors that indicate a predisposition toward chronic pain:
You know it at once. It may be the fiery sensation of a burn moments after your finger touches the stove. Or it’s a dull ache above your brow after a day of stress and tension. Or you may recognize it as a sharp pierce in your back after you lift something heavy. It is pain. In its most benign form, it warns us that something isn’t quite right, that we should take medicine or see a doctor. At its worst, however, pain robs us of our productivity, our well-being, and, for many of us suffering from extended illness, our very lives. Pain is a complex perception that differs enormously among individual patients, even those who appear to have identical injuries or illnesses. In 1931, the French medical missionary Dr. Albert Schweitzer wrote, “Pain is a more terrible lord of mankind than even death itself.” Today, pain has become the universal disorder, a serious and costly public health issue, and a challenge for family, friends, and health care providers who must give support to the individual suffering from the physical as well as the emotional consequences of pain. A Brief History of Pain Ancient civilizations recorded on stone tablets accounts of pain and the treatments used: pressure, heat, water, and sun. Early humans related pain to evil, magic, and demons. Relief of pain was the responsibility of sorcerers, shamans, priests, and priestesses, who used herbs, rites, and ceremonies as their treatments. The Greeks and Romans were the first to advance a theory of sensation, the idea that the brain and nervous system have a role in producing the perception of pain. But it was not until the Middle Ages and well into the Renaissance-the 1400s and 1500s-that evidence began to accumulate in support of these theories. Leonardo da Vinci and his contemporaries came to believe that the brain was the central organ responsible for sensation. Da Vinci also developed the idea that the spinal cord transmits sensations to the brain. In the 17th and 18th centuries, the study of the body-and the senses-continued to be a source of wonder for the world’s philosophers. In 1664, the French philosopher René Descartes described what to this day is still called a “pain pathway.” Descartes illustrated how particles of fire, in contact with the foot, travel to the brain and he compared pain sensation to the ringing of a bell. In the 19th century, pain came to dwell under a new domain – science – paving the way for advances in pain therapy. Physician-scientists discovered that opium, morphine, codeine, and cocaine could be used to treat pain. These drugs led to the development of aspirin, to this day the most commonly used pain reliever. Before long, anesthesia-both general and regional-was refined and applied during surgery. “It has no future but itself,” wrote the 19th century American poet Emily Dickinson, speaking about pain. As the 21st century unfolds, however, advances in pain research are creating a less grim future than that portrayed in Dickinsons verse, a future that includes a better understanding of pain, along with greatly improved treatments to keep it in check. The Two Faces of Pain: Acute and Chronic What is pain? The International Association for the Study of Pain defines it as: An unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage. It is useful to distinguish between two basic types of pain, acute and chronic, and they differ greatly. We may experience pain as a prick, tingle, sting, burn, or ache. Receptors on the skin trigger a series of events, beginning with an electrical impulse that travels from the skin to the spinal cord. The spinal cord acts as a sort of relay center where the pain signal can be blocked, enhanced, or otherwise modified before it is relayed to the brain. One area of the spinal cord in particular, called the dorsal horn (see section on Spine Basics in the Appendix), is important in the reception of pain signals. The most common destination in the brain for pain signals is the thalamus and from there to the cortex, the headquarters for complex thoughts. The thalamus also serves as the brain’s storage area for images of the body and plays a key role in relaying messages between the brain and various parts of the body. In people who undergo an amputation, the representation of the amputated limb is stored in the thalamus. (For a discussion of the thalamus and its role in this phenomenon, called phantom pain, see section on Phantom Pain in the Appendix.) Pain is a complicated process that involves an intricate interplay between a number of important chemicals found naturally in the brain and spinal cord. In general, these chemicals, called neurotransmitters, transmit nerve impulses from one cell to another. There are many different neurotransmitters in the human body; some play a role in human disease and, in the case of pain, act in various combinations to produce painful sensations in the body. Some chemicals govern mild pain sensations; others control intense or severe pain. The body’s chemicals act in the transmission of pain messages by stimulating neurotransmitter receptors found on the surface of cells; each receptor has a corresponding neurotransmitter. Receptors function much like gates or ports and enable pain messages to pass through and on to neighboring cells. One brain chemical of special interest to neuroscientists is glutamate. During experiments, mice with blocked glutamate receptors show a reduction in their responses to pain. Other important receptors in pain transmission are opiate-like receptors. Morphine and other opioid drugs work by locking on to these opioid receptors, switching on pain-inhibiting pathways or circuits, and thereby blocking pain. Another type of receptor that responds to painful stimuli is called a nociceptor. Nociceptors are thin nerve fibers in the skin, muscle, and other body tissues, that, when stimulated, carry pain signals to the spinal cord and brain. Normally, nociceptors only respond to strong stimuli such as a pinch. However, when tissues become injured or inflamed, as with a sunburn or infection, they release chemicals that make nociceptors much more sensitive and cause them to transmit pain signals in response to even gentle stimuli such as breeze or a caress. This condition is called allodynia -a state in which pain is produced by innocuous stimuli. The body’s natural painkillers may yet prove to be the most promising pain relievers, pointing to one of the most important new avenues in drug development. The brain may signal the release of painkillers found in the spinal cord, including serotonin, norepinephrine, and opioid-like chemicals. Many pharmaceutical companies are working to synthesize these substances in laboratories as future medications. Endorphins and enkephalins are other natural painkillers. Endorphins may be responsible for the “feel good” effects experienced by many people after rigorous exercise; they are also implicated in the pleasurable effects of smoking. Similarly, peptides, compounds that make up proteins in the body, play a role in pain responses. Mice bred experimentally to lack a gene for two peptides called tachykinins-neurokinin A and substance P-have a reduced response to severe pain. When exposed to mild pain, these mice react in the same way as mice that carry the missing gene. But when exposed to more severe pain, the mice exhibit a reduced pain response. This suggests that the two peptides are involved in the production of pain sensations, especially moderate-to-severe pain. Continued research on tachykinins, conducted with support from the NINDS, may pave the way for drugs tailored to treat different severities of pain. Scientists are working to develop potent pain-killing drugs that act on receptors for the chemical acetylcholine. For example, a type of frog native to Ecuador has been found to have a chemical in its skin called epibatidine, derived from the frog’s scientific name, Epipedobates tricolor. Although highly toxic, epibatidine is a potent analgesic and, surprisingly, resembles the chemical nicotine found in cigarettes. Also under development are other less toxic compounds that act on acetylcholine receptors and may prove to be more potent than morphine but without its addictive properties. The idea of using receptors as gateways for pain drugs is a novel idea, supported by experiments involving substance P. Investigators have been able to isolate a tiny population of neurons, located in the spinal cord, that together form a major portion of the pathway responsible for carrying persistent pain signals to the brain. When animals were given injections of a lethal cocktail containing substance P linked to the chemical saporin, this group of cells, whose sole function is to communicate pain, were killed. Receptors for substance P served as a portal or point of entry for the compound. Within days of the injections, the targeted neurons, located in the outer layer of the spinal cord along its entire length, absorbed the compound and were neutralized. The animals’ behavior was completely normal; they no longer exhibited signs of pain following injury or had an exaggerated pain response. Importantly, the animals still responded to acute, that is, normal, pain. This is a critical finding as it is important to retain the body’s ability to detect potentially injurious stimuli. The protective, early warning signal that pain provides is essential for normal functioning. If this work can be translated clinically, humans might be able to benefit from similar compounds introduced, for example, through lumbar (spinal) puncture. Another promising area of research using the body’s natural pain-killing abilities is the transplantation of chromaffin cells into the spinal cords of animals bred experimentally to develop arthritis. Chromaffin cells produce several of the body’s pain-killing substances and are part of the adrenal medulla, which sits on top of the kidney. Within a week or so, rats receiving these transplants cease to exhibit telltale signs of pain. Scientists, working with support from the NINDS, believe the transplants help the animals recover from pain-related cellular damage. Extensive animal studies will be required to learn if this technique might be of value to humans with severe pain. One way to control pain outside of the brain, that is, peripherally, is by inhibiting hormones called prostaglandins. Prostaglandins stimulate nerves at the site of injury and cause inflammation and fever. Certain drugs, including NSAIDs, act against such hormones by blocking the enzyme that is required for their synthesis. Blood vessel walls stretch or dilate during a migraine attack and it is thought that serotonin plays a complicated role in this process. For example, before a migraine headache, serotonin levels fall. Drugs for migraine include the triptans: sumatriptan (Imitrix®), naratriptan (Amerge®), and zolmitriptan (Zomig®). They are called serotonin agonists because they mimic the action of endogenous (natural) serotonin and bind to specific subtypes of serotonin receptors. Ongoing pain research, much of it supported by the NINDS, continues to reveal at an unprecedented pace fascinating insights into how genetics, the immune system, and the skin contribute to pain responses. The explosion of knowledge about human genetics is helping scientists who work in the field of drug development. We know, for example, that the pain-killing properties of codeine rely heavily on a liver enzyme, CYP2D6, which helps convert codeine into morphine. A small number of people genetically lack the enzyme CYP2D6; when given codeine, these individuals do not get pain relief. CYP2D6 also helps break down certain other drugs. People who genetically lack CYP2D6 may not be able to cleanse their systems of these drugs and may be vulnerable to drug toxicity. CYP2D6 is currently under investigation for its role in pain. In his research, the late John C. Liebeskind, a renowned pain expert and a professor of psychology at UCLA, found that pain can kill by delaying healing and causing cancer to spread. In his pioneering research on the immune system and pain, Dr. Liebeskind studied the effects of stress-such as surgery-on the immune system and in particular on cells called natural killer or NK cells. These cells are thought to help protect the body against tumors. In one study conducted with rats, Dr. Liebeskind found that, following experimental surgery, NK cell activity was suppressed, causing the cancer to spread more rapidly. When the animals were treated with morphine, however, they were able to avoid this reaction to stress. The link between the nervous and immune systems is an important one. Cytokines, a type of protein found in the nervous system, are also part of the body’s immune system, the body’s shield for fighting off disease. Cytokines can trigger pain by promoting inflammation, even in the absence of injury or damage. Certain types of cytokines have been linked to nervous system injury. After trauma, cytokine levels rise in the brain and spinal cord and at the site in the peripheral nervous system where the injury occurred. Improvements in our understanding of the precise role of cytokines in producing pain, especially pain resulting from injury, may lead to new classes of drugs that can block the action of these substances.
Post Stroke Pain: is a pain the patient experiences immediately after a stroke. First, the pain sometimes occurs in the following weeks or months after a stroke. As such there are two different types of stoke pain: Following a stroke, the brain cannot comprehend the nerves signals sent by the body including reaction to touch, warmth, cold and others. The body now understands these as hurtful things. Consequently, symptoms of this condition include non-stop pain, repeating pain, the pain felt on the affected side of the body, pain in the face, legs, arms or torso, and throbbing/hot/stinging pain. As a result, individuals may stop moving painful body parts allowing their muscles to become lethargic. Treatments for pain following a stroke are: Consequently what kinds of pain might I feel after stroke? Headache These are more common after hemorrhagic stroke than ischaemic stroke. Consequently, it is not always known what causes headaches, but it can sometimes be a side effect of medications. Consequently, your doctor is the best person to determine if medication may help with your pain. Sometimes medications prescribed by your doctor will interact with other medications including over-the-counter medications or herbal remedies. As such it is important that you talk to your doctor or pharmacist about all the medications you are taking. This includes natural remedies or vitamin supplements. There are many types of medications that may help depending on the type of pain you feel. Such as:
Shoulder pain and other musculoskeletal problems
Pharmacological Management
Non-Pharmacological Management

Complex regional pain syndrome (CRPS) is a chronic (lasting greater than six months) pain condition that most often affects one limb (arm, leg, hand, or foot) usually after an injury. The peripheral nervous system involves nerve signaling from the brain and spinal cord to the rest of the body. CRPS is characterized by prolonged or excessive pain and changes in skin color, temperature, and/or swelling in the affected area. CRPS symptoms vary in severity and duration, although some cases are mild and eventually go away. In more severe cases, individuals may not recover and may have long-term disability. Although it is more common in women, CRPS can occur in anyone at any age, with a peak at age 40. CRPS is rare in the elderly. Very few children under age 10 and almost no children under age 5 are affected. The key symptom is prolonged severe pain that may be constant. It has been described as “burning,” “pins and needles” sensation, or as if someone were squeezing the affected limb. The pain may spread to the entire arm or leg, even though the injury might have only involved a finger or toe. In rare cases, pain can sometimes even travel to the opposite extremity. There is often increased sensitivity in the affected area, known as allodynia, in which normal contact with the skin is experienced as very painful. People with CRPS also experience changes in skin temperature, skin color, or swelling of the affected limb. This is due to abnormal microcirculation caused by damage to the nerves controlling blood flow and temperature. As a result, an affected arm or leg may feel warmer or cooler compared to the opposite limb. The skin on the affected limb may change color, becoming blotchy, blue, purple, pale, or red. Other common features of CRPS include: It is unclear why some individuals develop CRPS while others with similar trauma do not. CRPS represents an abnormal response that magnifies the effects of the injury. Peripheral nerve abnormalities found in individuals with CRPS usually involve the small unmyelinated and thinly myelinated sensory nerve fibers (axons) that carry pain messages and signals to blood vessels. (Myelin is a mixture of proteins and fat-like substances that surround and insulate some nerve fibers.) Because small fibers in the nerves communicate with blood vessels, injuries to the fibers may trigger the many different symptoms of CRPS. Molecules secreted from the ends of hyperactive small nerve fibers are thought to contribute to inflammation and blood vessel abnormalities. These peripheral nerve abnormalities in turn trigger damage in the spinal cord and brain. Blood vessels in the affected limb may dilate (open wider) or leak fluid into the surrounding tissue, causing red, swollen skin. The dilation and constriction of small blood vessels are controlled by small nerve fiber axons as well as chemical messengers in the blood. The underlying muscles and deeper tissues can become starved of oxygen and nutrients, which causes muscle and joint pain as well as damage. The blood vessels may over-constrict (clamp down), causing old, white, or bluish skin. CRPS also affects the immune system. High levels of inflammatory chemicals (cytokines) have been found in the tissues of people with CRPS. These contribute to the redness, swelling, and warmth reported by many patients. CRPS is more common in individuals with other inflammatory and autoimmune conditions such as asthma. Limited data suggest that CRPS also may be influenced by genetics. Rare family clusters of CRPS have been reported. Familial CRPS may be more severe with earlier onset, greater dystonia, and more than one limb being affected. Occasionally CRPS develops without any known injury. In these cases, an infection, a blood vessel problem, or entrapment of the nerves may have caused an internal injury. A physician will perform a thorough examination in order to identify a cause. In many cases, CRPS results from a variety of causes. In such instances, treatments are directed at all of the contributing factors. Currently, there is no specific test that can confirm CRPS. Since other conditions can cause similar symptoms, careful examination is important. As most people improve gradually over time, the diagnosis may be more difficult later in the course of the disorder. The outcome of CRPS is highly variable. Younger persons, children, and teenagers tend to have better outcomes. While older people can have good outcomes, there are some individuals who experience severe pain and disability despite treatment. Rehabilitation and physical therapy. An exercise program to keep the painful limb or body part moving can improve blood flow and lessen the circulatory symptoms. Additionally, exercise can help improve the affected limb’s flexibility, strength, and function. Occupational therapy can help the individual learn new ways to work and perform daily tasks. Psychotherapy. People with CRPS may develop depression, anxiety, or post-traumatic stress disorder, all of which heighten the perception of pain and make rehabilitation efforts more difficult. Treating these secondary conditions is important for helping people cope and recover from CRPS. All drugs or combination of drugs can have various side effects such as drowsiness, dizziness, increased heartbeat, and impaired memory. Inform a healthcare professional of any changes once drug therapy begins. Sympathetic nerve block. Sympathetic blocks involve injecting an anesthetic next to the spine to directly block the activity of sympathetic nerves and improve blood flow. Surgical sympathectomy. The use of this operation that destroys some of the nerves is controversial. Some experts think it is unwarranted and makes CRPS worse, whereas others report a favorable outcome. Spinal cord stimulation. Placing stimulating electrodes through a needle into the spine near the spinal cord provides a tingling sensation in the painful area. Electrodes may be placed temporarily for a few days in order to assess whether stimulation is likely to be helpful. Approximately 25 percent of individuals develop equipment problems that may require additional surgeries. Other types of neural stimulation. These include near injured nerves (peripheral nerve stimulators), outside the membranes of the brain (motor cortex stimulation with dural electrodes), and within the parts of the brain that control pain (deep brain stimulation). A recent option involves the use of magnetic currents applied externally to the brain (known as repetitive Transcranial Magnetic Stimulation, or rTMS). Intrathecal drug pumps. These devices pump pain-relieving medications directly into the fluid that bathes the spinal cord, typically opioids, local anesthetic agents, clonidine, and baclofen. There are no studies that show benefit specifically for CRPS. Intravenous immunoglobulin (IVIG). Researchers in Great Britain report low-dose IVIG reduced pain intensity in a small trial of 13 patients with CRPS for 6 to 30 months who did not respond well to other treatments. Those who received IVIG had a greater decrease in pain scores than those receiving saline during the following 14 days after infusion. Options include behavior modification, acupuncture, relaxation techniques (such as biofeedback, progressive muscle relaxation, and guided motion therapy), and chiropractic treatment.What is complex regional pain syndrome?
Who can get CRPS?
What are the symptoms of CRPS?
What causes CRPS?
Genetics & CRPS
Drugs to treat CRPS include:
Types of Drug Therapy
Emerging treatments for CRPS include:
Ketamine. Investigators are using low doses of ketamine—a strong anesthetic—given intravenously for several days to either reduce substantially or eliminate the chronic pain of CRPS.
Graded Motor imagery. Several studies have demonstrated the benefits of graded motor imagery therapy for CRPS pain. Individuals do mental exercises including identifying left and right painful body parts while looking into a mirror and visualizing moving those painful body parts without actually moving them.
What is carpal tunnel syndrome?
Carpal tunnel syndrome is numbness, tingling, weakness, and other problems in your hand because of pressure on the median nerve in your wrist.
The median nerve and several tendons run from your forearm to your hand through a small space in your wrist called the carpal tunnel. The median nerve controls movement and feeling in your thumb and first three fingers (not your little finger).
Cancer-related pain is a pain that develops from many different factors. From the medications one takes to cancer itself, the list of factors can vary. The patient experiences pain as individual as the person. Consequently, the pain experienced is dependent upon several different factors.
Arthritis is very common but is not well understood. Actually, “arthritis” is not a single disease; it is an informal way of referring to joint pain or joint disease. There are more than 100 different types of arthritis and related conditions. People of all ages, sexes, and races can and do have arthritis, and it is the leading cause of disability in America. More than 50 million adults and 300,000 children have some type of arthritis. It is most common among women and occurs more frequently as people get older.
What is ADD / ADHD?
ADD (attention-deficit disorder) or ADHD (attention-deficit/hyperactivity disorder) is a common condition that affects both children and adults, and symptoms can take a severe toll on the quality of life for sufferers, and their family and friends.